What?
Clinical breast examination (CBE) is when a doctor or a nurse examines the breasts and helps find lumps that women may miss with their own self-exams.
While it's true that most lumps are found by women themselves, the abnormality in a breast can be so difficult to feel that only someone with experience would recognize it. Lumps, thickening, asymmetry—changes in your breasts that you may not notice or think are "normal"—may be detected by a doctor who examines many breasts regularly. Studies show that regular self-exam, COMBINED with an annual exam by a doctor, improves the chances of detecting cancer early.
When?
Age 20 – 39
Do Breast Self-Examination (BSE) once a month, between the 7-10 day from the start of your period
Do Clinical Breast Examination (CBE) once every 3 years
Age 40 and above
Do monthly BSE. For women who have reached menopause, do it on a specific date of the month.
Do CBE and mammogram once a year
How?
CBE is done by a trained health professional, i.e. a doctor or a nurse. You will need to remove any jewelry that might interfere with the examination. You will need to take off your clothes above the waist, and you will be given a cloth or paper gown to wear during the examination.
First, the health professional will ask you questions about any symptoms you may have, your medical history, and your risk factors for breast cancer. Tell them if you:
- Have noticed a new lump or change in your breasts.
- Are or might be pregnant.
- Are breast-feeding.
- Have breast implants.
- Have previously had a breast biopsy.
- Have completed menopause.
- Are taking hormone replacement therapy.
- Have a personal or family history of breast cancer.
Your health professional will then examine each breast, underarm, and collarbone area for changes in breast size, skin changes, and signs of injury or infection, such as bruising or redness. You may be asked to lean forward and press your hands together to tighten the muscle beneath each breast during this part of the examination.
Your health professional will feel (palpate) each breast for any unusual or painful areas or a dominant lump. A dominant lump in the breast is any lump that is new, larger, harder, or different in any other way from other lumps or the rest of the breast tissue.
Your health professional will gently press on the breast tissue from about 1 in.(2.5 cm) below the breast up to the shoulder bone. He or she also will examine your armpit (axillary area) and your neck for swollen glands (lymph nodes).
A CBE normally does not cause any discomfort. If your breasts are tender because your menstrual period is about to begin, a CBE may cause slight discomfort when the health professional presses on your breasts to feel for lumps.
Findings of a CBE may include the following:
Clinical breast examination
Normal: The nipples, breast tissue, and areas around the breast are normal in size, shape, and appearance. One breast may be slightly larger than the other. A small area of firm tissue may be present in the lower curve of the breast below the nipple. Tenderness or lumpiness that occurs in both breasts and improves after a menstrual period is normal for many women. Many women have symmetrical lumpiness or thickening in both breasts throughout the menstrual cycle. A clear or milky discharge (galactorrhea) may be present when the nipple is squeezed. This may be caused by nursing, breast stimulation, hormones, or some other normal cause.
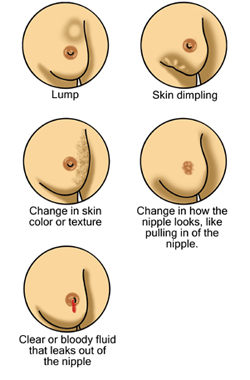
Abnormal: A firm lump or area of thickening may be present in one of your breasts.
Changes in the color or feel of your breast or nipple may be present. This can include wrinkling, dimpling, thickening, or puckering or an area that feels grainy, stringy, or thickened. A nipple may sink into the breast. A red, scaly rash or sore may be found on the nipple. Redness or warmth over a painful lump or over an entire breast may be present. This may be caused by an infection (abscess or mastitis) or cancer, such as inflammatory breast cancer. A bloody or milky discharge (galactorrhea) may occur without stimulation (spontaneous).
If a breast problem is found, the next step depends on the problem:
· Cyclic breast pain, fibrocystic changes, or cysts may just be rechecked to see whether they change or go away on their own. Cysts may also be examined by ultrasound or drained with a needle (aspirated) to make sure they are cysts and to help relieve pain.
· A mammogram or ultrasound may be ordered if a lump is found. Fluid may be drained if a cyst is present. Tissue for examination in the laboratory may be collected with a needle (needle aspiration or core biopsy) or through a small incision (biopsy).
· Nipple discharge, especially if it is spontaneous or bloody, may be examined under a microscope for unusual cells.